Procedure for Prolapse and Hemorrhoids (PPH)
Also known as the PPH procedure, stapled hemorrhoidectomy, stapled hemorrhoidopexy, and circumferential mucosectomy.
PPH is a technique developed in the early 90's that reduces the prolapse of hemorrhoidal tissue by excising a band of the prolapsed anal mucosa membrane with the use of a circular stapling device. In PPH, the prolapsed tissue is pulled into a device that allows the excess tissue to be removed while the remaining hemorrhoidal tissue is stapled. This restores the hemorrhoidal tissue back to its original anatomical position.
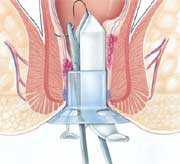
The introduction of the Circular Anal Dilator causes the reduction of the prolapse of the anal skin and parts of the anal mucous membrane. After removing the obturator, the prolapsed mucous membrane falls into the lumen of the dilator.

The Purse-String Suture Anoscope is then introduced through the dilator.
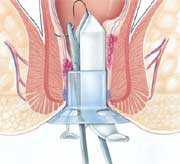
This anoscope will push the mucous prolapse back against the rectal wall along a 270° circumference, while the mucous membrane that protrudes through the anoscope window can be easily contained in a suture that includes only the mucous membrane. By rotating the anoscope, it will be possible to complete a purse-string suture around the entire anal circumference.
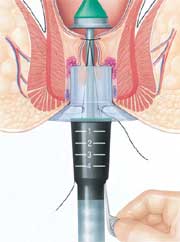
The Hemorrhoidal Circular Stapler is opened to its maximum position. Its head is introduced and positioned proximal to the purse-string, which is then tied with a closing knot.
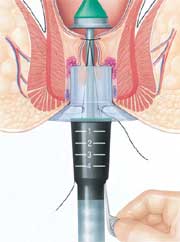 
The ends of the suture are knotted externally. Then the entire casing of the stapling device is introduced into the anal canal. During the introduction, it is advisable to partially tighten the stapler.

With moderate traction on the purse-string, a simple maneuver draws the prolapsed mucous membrane into the casing of the circular stapling device. The instrument is then tightened and fired to staple the prolapse. Keeping the stapling device in the closed position for approximately 30 seconds before firing and approximately 20 seconds after firing acts as a tamponade, which may help promote hemostasis.

Firing the stapler releases a double staggered row of titanium staples through the tissue. A circular knife excises the redundant tissue. A circumferential column of mucosa is removed from the upper anal canal. Finally, the staple line is examined using the anoscope. If bleeding from the staple line occurs, additional absorbable sutures may be placed. |



 The typical morphological situation of the hemorrhoidal and mucous prolapse is caused by weakening and breakage of the supporting muscular and connective fibers. Prolapse implies the distal dislocation of the internal hemorrhoidal cushions that push the external hemorrhoidal sacs in an outward and lateral direction, thus causing the sacs to protrude. The upper hemorrhoidal vessels extend, while the middle and lower hemorrhoidal vessels are subject to the formation of kinks. The hemorrhoidal volume may remain normal or swell due to phlebostasis. It may also regress towards atrophy. In IV degree prolapse, the dentate line is positioned almost outside the anal canal, and the rectal mucous membrane permanently occupies the muscular anal canal.
The typical morphological situation of the hemorrhoidal and mucous prolapse is caused by weakening and breakage of the supporting muscular and connective fibers. Prolapse implies the distal dislocation of the internal hemorrhoidal cushions that push the external hemorrhoidal sacs in an outward and lateral direction, thus causing the sacs to protrude. The upper hemorrhoidal vessels extend, while the middle and lower hemorrhoidal vessels are subject to the formation of kinks. The hemorrhoidal volume may remain normal or swell due to phlebostasis. It may also regress towards atrophy. In IV degree prolapse, the dentate line is positioned almost outside the anal canal, and the rectal mucous membrane permanently occupies the muscular anal canal.